Grass Roots Efforts to Battle the Opioid Crisis
Two recent news stories show that there are many ways of battling the opioid crisis. Former BC Minister for Health, Terry Lake, has recently stated he believes that marijuana could play a part in harm reduction, and could help people come off opioids. The Roshni Clinic is a medical clinic in BC and a social services office in Alberta working to provide support to those in the South Asian community affected by drugs and alcohol. Marijuana an Option for Opioid Reduction? Terry Lake was the Health Minister for BC during the time of declaring a public health emergency amid the fentanyl crisis and is now working as a vice president at a Quebec based medical cannabis company. He says further research is required, but some preliminary studies show that marijuana can help those with opioid addictions. Some studies have looked at reduced opioid death rates in US states that have legalized marijuana. A Canadian paper on medical cannabis patients showed that there was 63% decrease in prescription drug use and 30% decrease in opiate use. South Asian Focused Clinic Helping Opioid Users Fraser Health, one of BC’s health authorities, has opened The Roshni Clinic in response to the need for culturally sensitive care and services in Punjab and Hindi. Thirty percent of the population in Surrey, BC is Punjabi speaking. Often people need to bring along family members to act as translators, which is not always ideal. Alberta provided more than half a million dollars to increase funding to the Punjabi Community Health Services in Calgary and it is hoped that the BC government will increase their commitment. In the Alberta office, they are focusing on providing culturally tailored counselling, as well as distributing naloxone kits. The Roshni Clinic is part of the existing South Asian Clinic at the Jim Pattison Outpatient Care and Surgery Centre in Surrey. There they offer a number of services including medical management of withdrawal symptoms, individual counselling, relapse prevention, and group and family education. Looking at South Asian communities across Canada, the CEO of Punjabi Community Health Services in Ontario, Baldev Mutta, sees the opioid addiction taking root in truck and taxi drivers. These men are offered thousands of dollars to transport drugs across the country. This can lead to forming an addiction as they need to take these stimulants to meet the extreme deadlines. Sometimes it happens the other way around. They are pressured into taking stimulants by other drivers and end up becoming drug runners to pay for their addiction. Either way, expanding resources and reducing the stigma within the community will hopefully help curb the opioid addiction crisis. References: Ex BC Health Minister says pot a Promising Substitute for Opioid Addiction Clinics Across Canada Expanding Addiction Support for South Asian Families Specialized Help Available for South Asians on Opioids Fraser Health Opens New Substance Use Clinic to Support South Asian Community The post Grass Roots Efforts to Battle the Opioid Crisis appeared first on Canada Drug...
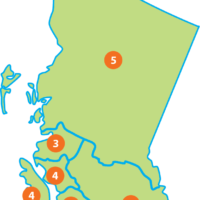
Provincial Snapshot: Accessing Public Treatment in BC
As part of our new series, Provincial Snapshot, Canada Drug Rehab will investigate the steps involved in how to access public treatment going from province to province each month. In Canada, you must be seeking treatment in the same province or territory as your health card. Only in rare cases can someone be referred across provincial lines. Therefore, if you are living in British Columbia and wish to seek treatment but are originally from Alberta, you must decide to either go back to Alberta for treatment or change over your health number/care card number to BC in order to receive treatment in BC. This month, we are starting with a look at British Columbia, the different health authorities in the province, and the best way to access publicly funded treatment. If you or someone you know requires urgent help, please call 911. Mental Health and Substance Use Services: Your Starting Point In order to receive public treatment in BC, you must start by calling or visiting one of the many mental health and substance use services offices. All major cities and most large towns have an office. First, find out which health authority you live in; this will help you find your closest office. There are 5 main health authorities in BC listed below and each is linked to the list of mental health and substance use offices found in that authority: Interior Health Authority (IHA) Fraser Valley Health Authority (FVH) Vancouver Coastal Health Authority (VCH) Vancouver Island Health Authority (VIHA) Northern Health Authority (NHA) These offices are responsible for the assessment of necessary services. Those struggling with addiction will be assessed to see if they need detox, outpatient help, inpatient services, etc. The office can also help with referrals to alternate programs and options ie. detox, rehab. At these offices, families can receive support and education on substance use issues. Those looking for help can also receive outpatient treatment, one-on-one counseling, and group programs. There is one other health authority that spans the entire province. The First Nations Health Authority (FNHA) allows for those with a valid status card to attend First Nations specific treatment programs within the province. Indigenous individuals can find their local FNHA office here. Some Improvements in Access The two health authorities in the Lower Mainland, FHA and VCH, have a “no barriers to access” policy. This policy has come about due to the opioid epidemic hitting the area hard. It means that those looking for help are no longer required to be a certain number of days sober before seeking treatment. This is in an attempt to battle the overdose deaths the area has been experiencing, and hopefully speed up the process to recovery. The bulk of the province’s population is in this area, therefore the majority of folks with substance use issues live here too. It is this reasoning that has meant that the rest of the province does NOT have this policy in place. Folks living in VIHA, NHA, and IHA must all meet whatever sobriety requirements their community’s specific office requires. However, some major centres like Prince George, Kelowna, Victoria, and Nanaimo can offer additional addiction resources not found in smaller towns in those regions. Inpatient/Residential Treatment (aka Rehab) Currently, Northern Health has no primary publicly funded residential program for adults. Therefore, all patients have to be referred to other health authorities, budget pending. Patients must participate in outpatient sessions within NHA in order for their application to be considered and referred onward. It is also contingent on the receiving health authority having the money and space for a new...
New Year New Hobbies: Substance-Free Activities to Try
Winter is well and truly here in western Canada. Snow is blanketing the towns and the days are getting longer, but still short. If you find it harder to maintain sobriety during winter now that there are fewer things to occupy your time, you are not alone. With these long dark evenings, many folks start to get ‘cabin fever’ from being confined to the house for months on end. So for this blog, we’ve highlighted three new hobbies to try out this winter, and maybe a few of them will even stick! Curling A classic Canadian past-time, in many towns, community life is centered around the rink. Curling is a great way to get out of the house and meet new people without being in a bar. Curling started as a way to alleviate the tedium of long winters so it only makes sense to put it on your list to try. No matter the size of the town almost all places in Canada have a curling rink and therefore a curling club. Joining a curling club means you are creating a new community for yourself, and making a commitment to show up for practices and tournaments. Being accountable to others can help you stay on top of the recovery commitments you’ve made to yourself. Crochet / Knitting Working with wool sounds like something for your grandma, but don’t let the stereotypes deter you. Crafting can be an affordable and satisfying hobby. Have a friend’s birthday coming up? Try knitting a basic scarf. It’s the easiest project to start with and it is the gift that truly keeps on giving. Your friend has a new scarf, you learned a new skill, your hands were busy, and your mind focused on your stitches. You also probably saved money on that gift by making it yourself! Yarn can be expensive at craft stores so head to a thrift store and you’ll be surprised at the large selection for a fraction of the cost. Hockey Like curling, hockey has become synonymous with Canada. Many kids grow up learning to skate and playing hockey. It may be one of your favourite sports to watch with friends at the bar or at someone’s house. This can be a tricky situation to get yourself into. You want to see your friends and watch something you love, however you don’t want to put yourself into a situation that is almost always full of beer. Joining an intramural hockey league can be a great way to combine your interests without the alcohol. References:http://www.curling.ca/foundation/2017/06/28/is-there-anything-more-canadian-than-curling/ https://www.quitterscircle.com/staying-smokefree/chew-on-this-the-need-to-engage-your-mouth-and-hands-after-quitting The post New Year New Hobbies: Substance-Free Activities to Try appeared first on Canada Drug...
Drug Fact Sheet: Ecstasy
Welcome to the first of our monthly drug fact sheets! A lot of us know the names of common recreational and prescription drugs, but do you know where they originated from, how they are produced, or what their effects really are? Each month we will take a look at a new substance and cover a few facts you should probably know about them. To kick off the new year we will be starting with Ecstasy and “party drugs”. While any drug you take while partying could be called a party drug, party drugs are usually substances that lead to loss of inhibition, lost sense of time and judgment, and a dissociative state that allows party goers to rave for hours without realizing a need to rest or nourish themselves. Therapeutic Origins of Ecstasy Ecstasy goes by many names including MDMA and Molly. True to its name, Ecstasy affects the part of the brain that controls mood and can make users feel very loving and happy go lucky. The chemical compound was patented back in 1913 by Merck, but after that they never pursued marketing or even produced it. Dr. Alexander Shulgin has been credited as the father of modern Ecstasy and other party drugs after he started tinkering with hallucinogens in the 1970s. He first synthesized and tried Ecstasy in 1976 and while many blame him for it gaining such traction in the 1980s, he had always intended it to be used therapeutically. He sent samples to therapists to try with their patients and recorded their observations. However, just 10 years after he first experienced Ecstasy, the drug had made its way into so many nightclubs and there were so many bad reactions due to backyard chemists and dealers that the DEA put Ecstasy on its Schedule 1 list of dangerous drugs. Ecstasy, like a lot of other party drugs, may have started out rather innocuously but became potentially very dangerous due to the illegal drug trade. In the original rave days, Molly was supposed to be an even purer form of Ecstasy as it was exclusively MDMA (methylendioxymethamphetamine) the active ingredient in Ecstasy. However, today you can never be sure what your drugs are cut with, and many police seizures of pills show there is no MDMA at all in most pills being marketed as Ecstasy. In the late 2000s, only 13% of the Molly seized by the DEA in New York contained MDMA and even then it was still cut with other toxic chemicals. References: http://www.narconon.ca/drug-information/ecstasy-history.html http://www.latimes.com/local/obituaries/la-me-alexander-shulgin-20140605-story.html https://globalnews.ca/news/1603229/what-is-party-drug-molly/ http://www.cnn.com/2013/11/22/health/9-things-molly-drug/index.html http://www.healthcommunities.com/substance-abuse/drugs.shtml The post Drug Fact Sheet: Ecstasy appeared first on Canada Drug...
Gaming Addiction now a WHO Designated Disorder
The World Health Organization (WHO) has begun 2018 by adding “gaming disorder”, or gaming addiction, to its International Classification of Diseases (ICD). This comes after years of rumblings by health professionals noting addictive behaviours exhibited in some video gamers. The Diagnostic and Statistical Manual of Mental Disorders (DSM) is the “bible” of psychiatric disorders. In 2013, the most recent edition of the DSM listed internet gaming disorder as a “condition for further study”. This shows how much traction this concept has gained over the last five years to now officially list it as a disorder. Gaming is a process addiction, like gambling and sex addiction. This means a person has an addiction to doing something rather than consuming something. A substance addiction is when consuming things like drugs and alcohol becomes a compulsion. The WHO report outlines many specifics that must be considered before a person can be diagnosed with gaming disorder. Their desire to play video games must overtake the need to do other important activities in their daily life. This kind of behaviour should also be observed for at least a year before a diagnosis is given. Emotional signs of video game addiction can look like isolation from friends and family so the person can spend more time gaming, and irritability when unable to play. These kinds of emotional signs are common across addiction types. Gaming disorder also has physical symptoms like carpal tunnel syndrome from overuse of controllers or keyboard and mouse, poor hygiene as they spend more time in the game, and headaches from the artificial screen light. It is hoped by gaming addiction being classified as a disorder, those who suffer can have better access to treatment options. Those with a gaming disorder must not be shamed or laughed off just because it is a new diagnosis. As a society, we have recognized some people’s predisposition for excessive gambling for centuries. Therefore, this process addiction is just a sign of our modern era and the new vices available to people. Even prior to the WHO’s announcement there were countries who had independently declared gaming addiction as a disorder. There are many private treatment facilities that are already operational and aim to treat this disorder. In countries that had not yet added this classification, the WHO declaration will make it easier for public funding to become available and provide avenues for proper medical treatment plans. References: https://www.sunshinecoasthealthcentre.ca/2015/06/process-addiction/ http://www.bbc.com/news/technology-42541404 https://www.psychguides.com/guides/video-game-addiction-symptoms-causes-and-effects/ The post Gaming Addiction now a WHO Designated Disorder appeared first on Canada Drug...